What is prolotherapy?
Prolotherapy or ligament regeneration therapy is a treatment for tendon and ligament injuries. Prolotherapy initiates new growth in weak tendons and ligaments. It can be used to treat several types of musculoskeletal pain. It can also help heal joints, ligaments, tendons, or other connective tissues when other therapies no longer help.
The ligaments hold the bones together. Wear or accident can damage, elongate or weaken the ligaments. Healing of damaged ligaments is a slow process and does not always lead to full recovery nor does it regain their original strength. Damaged ligaments can cause pain (eg ankle injury) and joint instability, accelerating joint aging.
Tendons are similar to ligaments, only tendons connect muscles to bones. Tendons can also be damaged and cause pain (e.g., tennis elbows) and result in poor muscle function.
How does prolotherapy work?
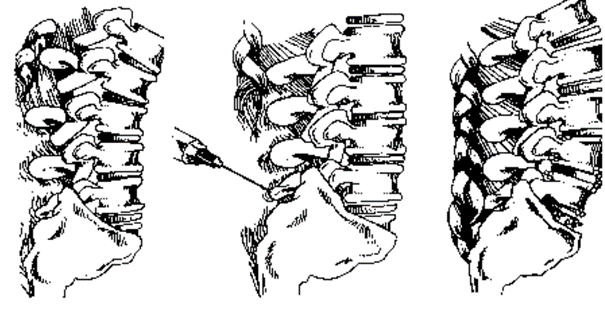
Prolotherapy involves several injectable treatments that elicit a controlled, local inflammatory response, similar to recovery from normal injury. As a result, new tissues begin to grow.
At our clinic, our goal is to restore the body’s healthy locomotor function, reduce pain, and improve patients ’daily lives. Through tissues reinforced by prolotherapy, and with a reduction in pain, other therapies (physiotherapy) are likely to be more effective, even if they have failed in the past.
We recommend to pair prolotherapy with:
• treating myofascial (muscle) pain: for example, massage, shock wave therapy – direct treatment of the origin of the pain
• physiotherapy and exercise
• lifestyle changes such as increased activity, a healthy diet and satisfactory sleep.
What does the treatment involve?
During prolotherapy, a solution containing a local anesthetic and dextrose (sugar) is injected into the joints, ligaments or tendons to stimulate tissue regeneration, triggering a reaction similar to normal healing. One treatment usually involves several injections.
Most patients require 3-8 treatments depending on the area being treated, the extent of the injury, and the rate of tissue healing. Treatments should be performed every 2-6 weeks.
It may take a few months for the tendons and ligaments to heal completely, but most patients usually report significant improvement after treatment 3 or 4. After completing therapy, patients often improve for months.
How do you know if prolotherapy will help?
Physicians at the Pain Clinic will first assess the patient’s condition and then, if they deem it necessary, will only recommend prolotherapy.
How long will the pain relief last?
Results may vary from patient to patient. If we eliminate instability with prolotherapy and exercise and treat the cause of the pain (strengthen the ligaments of the joints and tendons), the pain may even go away permanently. If the underlying cause cannot be eliminated (eg, previous lamellar spinal fusion or injury due to repeated exertion), symptoms usually improve but may recur later.
In some patients, we may not be able to get results with prolotherapy. This is usually known after the third treatment, in which case we choose a different therapeutic route.
Possible side effects
As with most medicine, some patients may experience side effects while others may not. The doctor will inform the patient about the possible risks.
Possible side effects
Common, mild side effects:
• Increased tenderness and swelling of the muscles and joints (for patients with a stronger reaction, less treatment is usually enough), which lasts for an average of 2-3 days, sometimes max. They last for 10 days.
Rare side effects:
• Bruising symptoms
Very rare side effects
• Fever. The patient may experience febrile symptoms on the first day after treatment. Fever 24 hours after treatment may indicate an infection that can be treated with antibiotics.
Potential risks
Prolotherapy does not worsen the patient’s condition in the long term, unless there is any complication from the puncture during the procedure.
These typically include bleeding, infection, and an allergic reaction to the administered solution.
Other complications depend on the current area being treated, such as:
Hips, knees, ankles, shoulders, elbows, wrists:
Nerve injury, vascular injury
Cervical, dorsal and lumbar spine:
Low blood pressure, chest tightness, spinal headache, nerve damage, vascular damage
paralysis, death.
To avoid these complications, we perform higher-risk punctures in our facility under ultrasound and / or X-ray control.
How can you prepare for prolotherapy treatment?
- Anti-inflammatory drugs should be discontinued 2 weeks before treatment. These include: Aspirin, Naproxen, Ibuprofen, Diclofenac, Chinese anti-inflammatory teas, etc.
- Smoking can reduce the effectiveness of therapy, so we recommend that you quit smoking.
- The patient should be accompanied.
- Treatment is usually in mild sedation, so you should eat and drink for the last time 6 hours before the procedure.
- Water should be consumed 2 hours before the procedure. Subsequent sedation may be omitted if required by the patient.
What to do after the treatment?
After treatment, the patient can resume all normal activities, but be careful not to strain. It is important to start physiotherapy and physiotherapy as soon as possible and to further increase the effectiveness of prolotherapy.
It is recommended to take a healthy, high-protein diet and vitamin C (500mg daily).
No additional medicated analgesia is usually required, a warm or cold compress as needed, or gentle exercise is recommended.
If the patient still requires, Tramadol 50mg / 6 hours and paracetamol 500mg / 4-6 hours can be taken.
Source:
Prolotherapy in the Treatment of Sports-Related Tendinopathies
https://josr-online.biomedcentral.com/articles/10.1186/s13018-024-04754-4


